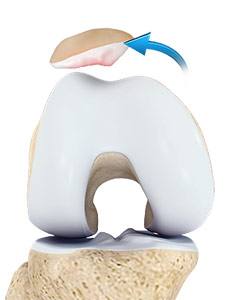
Anatomy of the Patella
The patella is a small piece of bone in front of the knee that slides up and down the groove in the femur bone during bending and stretching movements. The ligaments on the inner and outer sides of the patella hold it in the femoral groove and avoid dislocation of the patella from the groove.
What is Patellar Instability?
Any damage to the supporting ligaments may cause the patella to slip out of the groove either partially (subluxation) or completely (dislocation). This misalignment can damage the underlying soft structures such as muscles and ligaments that hold the kneecap in place. Once damaged, these soft structures are unable to keep the patella (kneecap) in position. Repeated subluxation or dislocation makes the knee unstable. This condition is called knee instability. Patellar (kneecap) instability results from one or more complete or partial dislocations (subluxations).
Symptoms of Patellar Instability
The signs and symptoms of patellar instability include:
- Pain, especially when standing up from a sitting position
- Feeling of unsteadiness or tendency of the knee to give way or buckle
- Recurrent subluxation
- Recurrent dislocation
- Severe pain, swelling and bruising of the knee immediately following subluxation or dislocation
- Visible deformity and loss of function of the knee, which often occurs after subluxation or dislocation
- Changes in sensations such as numbness or even partial paralysis, which can occur below the dislocation because of pressure on the nerves and blood vessels
Causes of Patellar Instability
Various factors and conditions may cause patellar instability. Often a combination of factors can cause this abnormal tracking and include the following:
- Anatomical defect: Flat feet or fallen arches and congenital abnormalities in the shape of the patella bone can cause misalignment of the knee joint.
- Abnormal “Q” Angle: The “Q” angle is a medical term used to describe the angle between the hips and knees. The higher the “Q” angle, such as in knock knees, the more the quadriceps pull on the patella, causing misalignment.
- Patellofemoral Arthritis: Patellar misalignment causes uneven wear and tear and can eventually lead to arthritic changes in the joint.
- Improper Muscle Balance: Quadriceps, the anterior thigh muscles, function to help hold the kneecap in place during movement. Weak thigh muscles can lead to abnormal tracking of the patella, causing it to subluxate or dislocate.
Diagnosis of Patellar Instability
Your surgeon diagnoses the condition by collecting your medical history and physical findings. He may also order certain tests such as X-rays, MRI or CT scans to confirm the diagnosis.
Treatment of Patellar Instability
The treatment for instability depends on the severity of the condition and is based on diagnostic reports. Initially, your surgeon may recommend conservative treatments such as physical therapy, use of braces and orthotics. Pain relieving medications may be prescribed for symptomatic relief. However, when these conservative treatments yield unsatisfactory response, surgical correction may be recommended.
Considering the type and severity of the injury, your surgeon decides on the surgical correction. A lateral retinacular release may be performed, where your surgeon releases or cuts the tight ligaments on the lateral side (outside) of the patella, enabling it to slide more easily in the femoral groove.
Your surgeon may also perform a procedure to realign the quadriceps mechanism by tightening the tendons on the inside or medial side of the knee.
If the misalignment is severe, tibial tubercle transfer (TTT) will be performed. This procedure involves removal of a section of bone where the patellar tendon attaches on the tibia. The bony section is then shifted and properly realigned with the patella and reattached to the tibia with two screws.
Following the surgery, a rehabilitation program may be recommended for better outcomes and quicker recovery.
Related Topics
- Patellar Instability
- Multiligament Instability
- Patellofemoral Instability
- Posterolateral Instability
- Knee Arthritis
- Knee Osteoarthritis
- Knee Injury
- Knee Pain
- Anterior Knee Pain
- Meniscal Tears
- Runners Knee
- Jumpers Knee
- Unstable Knee
- Knee Sprain
- MCL Sprains
- ACL Tears
- MCL Tears
- Meniscal Injuries
- PCL Injuries
- Ligament Injuries
- Knee Fracture
- Fractures of the Tibia
- Patella Fracture
- Tibial Shaft Fracture
- Kneecap Bursitis
- Chondral or Articular Cartilage Defects
- Quadriceps Tendon Rupture
- Patellar Tendon Rupture
- Lateral Meniscus Syndrome
- Osteonecrosis of the Knee
- Knee Angular Deformities
- Osteochondral Defect of the Knee
- Articular Cartilage Injury
- Goosefoot Bursitis of the Knee
- Iliotibial Band Syndrome
- Bowed Legs
- Recurrent Patella Dislocation
- Osteochondritis Dissecans of the Knee
- Chondromalacia Patella
- Patellar Tendinitis
- Knee Sports Injuries
- Multiligament Knee Injuries
- Women and ACL Injuries
- Medial Meniscus Syndrome
- Tibial Plateau Fracture
- Tibial Eminence Fractures
- Loose Bodies in the Knee
- Osgood Schlatter Disease
- Patellar Dislocation/Patellofemoral Dislocation